CardioTelligence
Headquarter Center
UAE, Duabi
Email Address
Cardiotelligence@gmail.com
Contact Number
(+98)9111861067
Cardiotelligence@gmail.com
This Study aims to investigate the clinical features and outcomes of cerebellitis post-COVID-19, providing insights for medical management. Here's a detailed interpretation of the study's statistical and professional aspects:
Study Design and Methods
Systematic Review and Data Sources: The researchers conducted a systematic search through multiple databases (PubMed, Web of Science, Embase, ProQuest, and Cochrane) for cases from January 2018 to September 2023. The inclusion criteria focused on case reports and series detailing cerebellitis following COVID-19 infection confirmed by brain imaging.
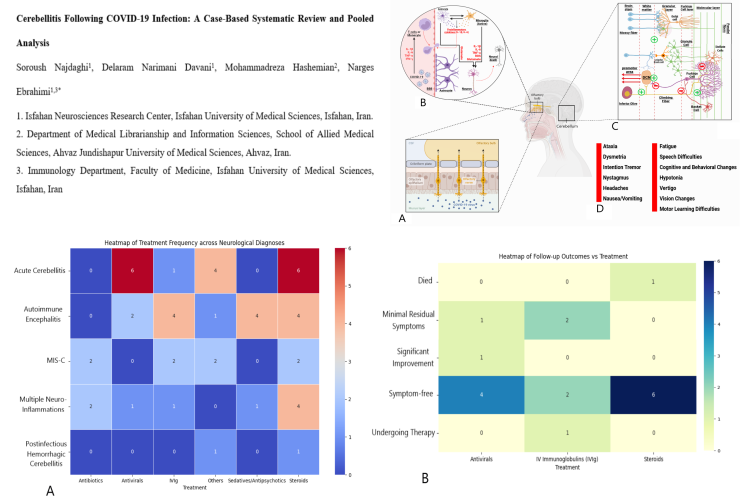
Data Analysis: Descriptive statistics were used to summarize demographics, clinical characteristics, and diagnostic techniques. Chi-Square tests assessed the associations between diagnoses, treatments, and outcomes. Visualizations such as heatmaps and scatter plots were utilized.
Results
Demographics and Patient Pro The analysis included 18 cases from 9 countries. The majority were from the USA (27.8%), with a mean patient age of 40.1 years (±24.6), and males comprised 94.4% of the cases. Common comorbidities included hypertension (22.2%) and diabetes (11.1%).
Symptom Onset: Neurological symptoms appeared on average 15.15 days (±12.7) post-COVID-19 infection. There was a moderate negative correlation (r = -0.358) between age and symptom onset, indicating younger individuals experienced symptoms sooner.
Biomarker Analysis: Blood and cerebrospinal fluid (CSF) biomarkers showed weak correlations with symptom onset intervals. Elevated blood CRP was noted in 33.3% of cases, and CSF protein levels were elevated in 50% of cases.
Imaging and Diagnosis: MRI was the preferred diagnostic modality, showing various cerebellar abnormalities. Ground-glass opacities were the most common pulmonary finding.
Treatment and Outcomes: Treatment efficacy varied, with a combination of antivirals and steroids yielding symptom-free outcomes in most cases. The Chi-Square test showed no significant statistical associations between diagnosis-treatment (p-value = 0.089) and follow-up outcomes (p-value = 0.283).
Statistical Insights
Chi-Square Tests: The p-values from the Chi-Square tests indicate that there were no significant associations between the types of treatments used and the neurological outcomes of the patients.
Correlation Coefficients: The Pearson correlation coefficients suggest a moderate relationship between age and the time to neurological symptom onset, but only weak correlations between blood/CSF biomarkers and symptom onset intervals.
Descriptive Statistics: Central tendency measures (mean, median) and dispersion (standard deviation, range) provided a comprehensive summary of the patient demographics and clinical characteristics.
Professional Implications
Clinical Features: The study highlights a higher incidence of cerebellitis in middle-aged males with vascular comorbidities. This information is crucial for clinicians to identify at-risk populations.
Diagnostic Techniques: MRI remains a key diagnostic tool for detecting cerebellar abnormalities post-COVID-19, emphasizing its importance in clinical settings.
Treatment Strategies: The combination of antivirals and steroids shows promise, but the lack of significant statistical associations suggests that more research is needed to establish standardized treatment protocols.
Biomarker Role: The weak correlations between biomarkers and symptom onset intervals indicate that while biomarkers can aid in diagnosis, they may not be reliable predictors of disease progression.
Study Design and Methods
Systematic Review and Data Sources: The researchers conducted a systematic search through multiple databases (PubMed, Web of Science, Embase, ProQuest, and Cochrane) for cases from January 2018 to September 2023. The inclusion criteria focused on case reports and series detailing cerebellitis following COVID-19 infection confirmed by brain imaging.
Data Analysis: Descriptive statistics were used to summarize demographics, clinical characteristics, and diagnostic techniques. Chi-Square tests assessed the associations between diagnoses, treatments, and outcomes. Visualizations such as heatmaps and scatter plots were utilized.
Results
Demographics and Patient Pro The analysis included 18 cases from 9 countries. The majority were from the USA (27.8%), with a mean patient age of 40.1 years (±24.6), and males comprised 94.4% of the cases. Common comorbidities included hypertension (22.2%) and diabetes (11.1%).
Symptom Onset: Neurological symptoms appeared on average 15.15 days (±12.7) post-COVID-19 infection. There was a moderate negative correlation (r = -0.358) between age and symptom onset, indicating younger individuals experienced symptoms sooner.
Biomarker Analysis: Blood and cerebrospinal fluid (CSF) biomarkers showed weak correlations with symptom onset intervals. Elevated blood CRP was noted in 33.3% of cases, and CSF protein levels were elevated in 50% of cases.
Imaging and Diagnosis: MRI was the preferred diagnostic modality, showing various cerebellar abnormalities. Ground-glass opacities were the most common pulmonary finding.
Treatment and Outcomes: Treatment efficacy varied, with a combination of antivirals and steroids yielding symptom-free outcomes in most cases. The Chi-Square test showed no significant statistical associations between diagnosis-treatment (p-value = 0.089) and follow-up outcomes (p-value = 0.283).
Statistical Insights
Chi-Square Tests: The p-values from the Chi-Square tests indicate that there were no significant associations between the types of treatments used and the neurological outcomes of the patients.
Correlation Coefficients: The Pearson correlation coefficients suggest a moderate relationship between age and the time to neurological symptom onset, but only weak correlations between blood/CSF biomarkers and symptom onset intervals.
Descriptive Statistics: Central tendency measures (mean, median) and dispersion (standard deviation, range) provided a comprehensive summary of the patient demographics and clinical characteristics.
Professional Implications
Clinical Features: The study highlights a higher incidence of cerebellitis in middle-aged males with vascular comorbidities. This information is crucial for clinicians to identify at-risk populations.
Diagnostic Techniques: MRI remains a key diagnostic tool for detecting cerebellar abnormalities post-COVID-19, emphasizing its importance in clinical settings.
Treatment Strategies: The combination of antivirals and steroids shows promise, but the lack of significant statistical associations suggests that more research is needed to establish standardized treatment protocols.
Biomarker Role: The weak correlations between biomarkers and symptom onset intervals indicate that while biomarkers can aid in diagnosis, they may not be reliable predictors of disease progression.
Are you Interested in Writing These Articles?
Join Us
